Peptic ulcer: how to identify by tests
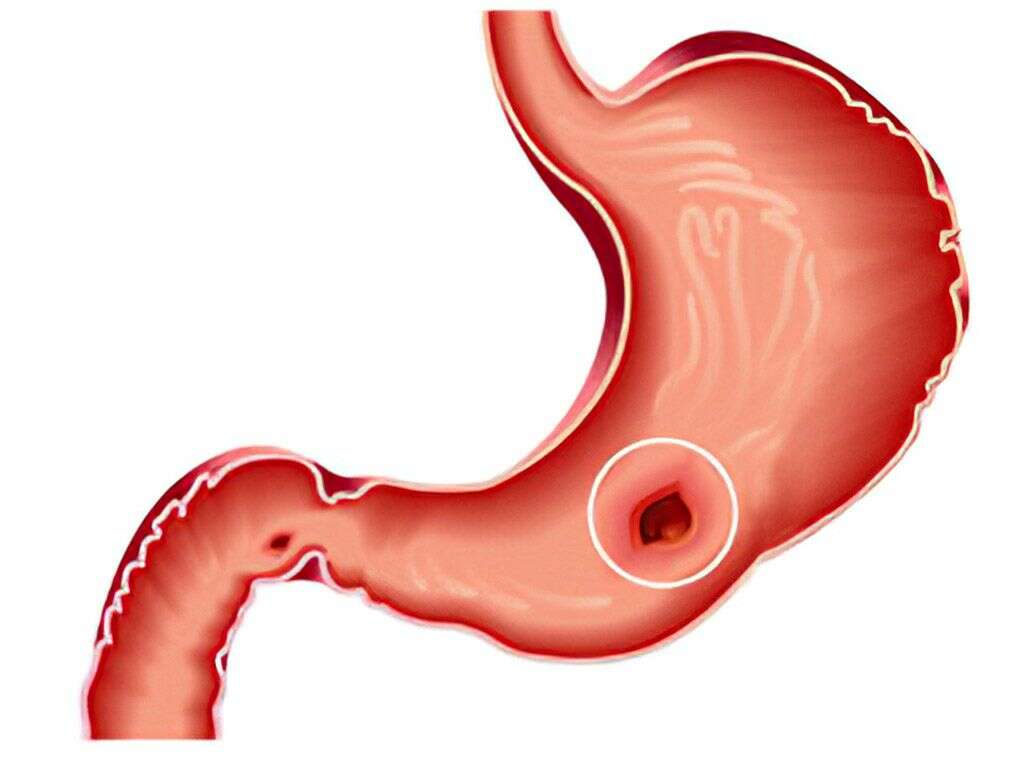
More recently, patients with suspected gastric or intestinal ulcers were forced to undergo a rather unpleasant procedure – FGDS. “Swallowing a light bulb,” as endoscopy is called in everyday life, was the only way to confirm or deny the diagnosis. And today – the risk of developing stomach ulcers can be “seen” by analyzes.
It may seem surprising, but changes in the mucous membrane of the stomach and duodenum can be “tracked” in a blood test. And for this you only need 4 markers.
Pepsinogen
Pepsinogen is a “dormant” form of pepsin – an enzyme that “disassembles” complex food proteins into “constituents” down to amino acids. And this “task” is so delicate and laborious that the stomach “has” to use not one, but two types of pepsinogen.
Pepsinogen-1 is synthesized by the cells of the upper half (bottom and body) of the stomach and passes into its active form (pepsin) at a very low pH of 1.5-2.0. Therefore, the main digestive functions of the stomach are realized here.
Sections remote from the “epicenter” of digestion, such as the passage of the esophagus into the stomach (cardiac section) and the stomach into the duodenum (antrum and pyloric section) no longer have such a low pH.
The fact is that the body and the fundus of the stomach, normally, are reliably protected from “corroding” by hydrochloric acid, which is produced by the cells of the stomach. Whereas the ingress of acid into the esophagus or 12-duodenum causes a burn of the mucous membrane. Which, in the case of the esophagus, feels like heartburn.
However, the degree of protein breakdown should be maximized before they enter the duodenum. And in order to involve all its departments in this “work”, the stomach produces another form of pepsinogen.
Pepsinogen-2 is converted to pepsin at higher pH values of about 4.5. And it works not only in the stomach, but also in the upper parts of the duodenum, where acidity has not yet reached alkaline values due to bile.
A decrease in pepsinogen-2 in the blood is associated with Helicobacter pylori infection and an increased risk of “gastric” oncology. A deficiency of pepsinogen-1 is a marker of atrophic gastritis of the gastric body, directly correlating with the severity of the lesion.
On the contrary, an increase in both indicators is associated with ulcerative lesions of the stomach and duodenum. And the ratio of both forms to each other has an important diagnostic value.
The decrease in the ratio of pepsinogen-1 to pepsinogen-2 reflects the severity of the inflammatory process and the degree of impairment in the production of enzymes. And the lower the number, the stronger the inflammation and the higher the risk of developing stomach cancer.
Gastrin
Gastrin is a gastric “hormone” that controls the synthesis of hydrochloric acid.
Normally, gastrin is activated only when food enters the stomach. And, like any hormone, it works according to the principle of “feedback”.
If there is not enough hydrochloric acid in the stomach, the level of gastrin rises in order to “spur” the cells to produce it.
If there is too much acid, the gastrin level drops.
A decrease in the indicator is observed with atrophic gastritis and increased acidity of the stomach. A decrease – with Helicobacter pylori infection, peptic ulcer and stomach cancer.
Antibodies IgG to H. pylori
The connection between Helicobacter pylori infection and gastric ulcer and 12-duodenal ulcer has been known for a long time. However, infection with a bacterium does not yet “guarantee” an ulcer.
According to modern research, in most of the infected, the immune system successfully “copes” with the pathogen. But about 15-20% develop a peptic ulcer.
It is assumed that this is due to the genetic characteristics of immunity, however, it has not yet been possible to accurately prove the theory.
Therefore, today, an increase in IgG antibodies to the Helicobacter bacterium is considered an important marker of risk (if there are no symptoms yet or they are weakly expressed) or the presence of stomach and duodenal ulcers.
Thus, the diagnosis of an ulcer https://en.wikipedia.org/wiki/Peptic_ulcer_disease by a blood test, due to its high accuracy and information content, is gaining more and more popularity among both patients and doctors. And this “Gastrocomplex” has already been “nicknamed” a serological biopsy.
More recently, patients with suspected gastric or intestinal ulcers were forced to undergo a rather unpleasant procedure – FGDS. “Swallowing a light bulb,” as endoscopy is called in everyday life, was the only way to confirm or deny the diagnosis. And today – the risk of developing stomach ulcers can be “seen” by analyzes. It…